Why foster kids in residential treatment do not ask for help?
|
Getting your Trinity Audio player ready...
|
On the resident’s point sheet, you will find a section called program participation: therapy worth 5 points. As a residential treatment counselor, the older youth that I worked with who was around 13 through 16 years old, didn’t know who their therapist was—let alone the option to speak to one. Specifically, the one assigned to them. Working in a residential treatment center, I had the therapist’s name and phone number who was assigned to each child, but as the children—I didn’t know their schedule or appointment for therapy.
On the weekend’s I would also see a per diem therapist walking through the cottage, but Monday through Wednesday (my work schedule) I never saw a therapist walk into the cottage (for around 9 months give or take). Towards the end of my experience, there was one therapist assigned to my cottage and was able to understand she was the therapist for most of the children (another therapist was assigned to a little boy that was transferred to my cottage but had a completely different therapist).
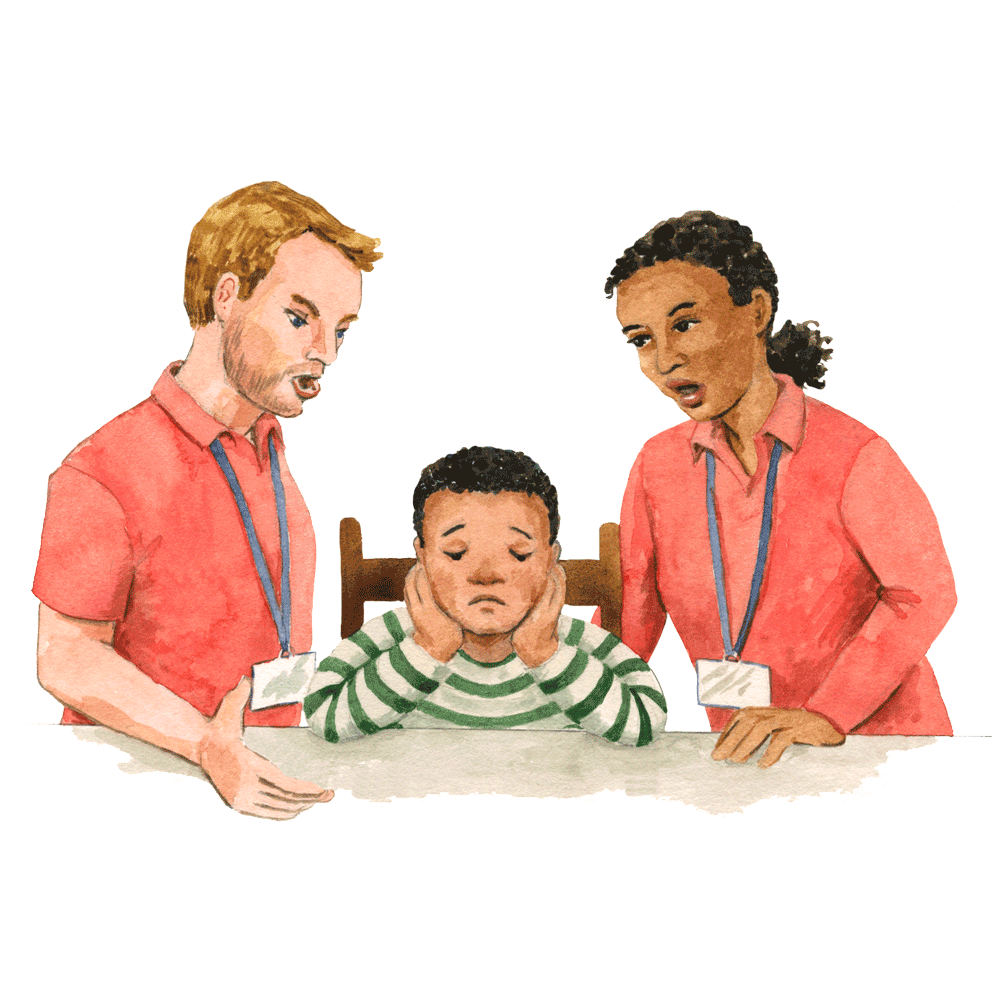
Depending on who was marking their point sheet, staff would dock points when residents did not ask to speak to their therapist. Now here is where I find the problem. While the staff is waiting on the youth to speak to their therapist. The therapist is waiting in their office until staff calls them into the cottage to do therapy or for the child to walk to their office.
The problem wasn’t the teens who refused or didn’t know therapy was a part of their point sheet or program. The problem was the treatment center’s direct care staff and therapists’ lack of communication with each other and to their patients—along with a number of other reasons we will discuss. The services and supports the youth received were ineffective because I believe the youth did not receive the services and supports they needed.
The department of mental health has no system in place that monitors, screens or researches congregate care outcomes or progress. These facilities can claim to help with their serious mental health concerns, education, aggression, substance abuse, and trauma, but while working in one— I never saw any services that provided quality mental health care, trauma support, academic support, and life skills for when the older boys aged-out of the treatment center. And since there’s no research, it’s hard to know what is or isn’t working. But when you look at how many youths become homeless (40-50%), enter the justice system (90% if they have 5+ more placements), and endure PTSD (double the rate of war veterans)— foster teens in congregate care are crying out for better services!
What they really do get in a therapeutic treatment center:
- 3 meals a day
- 2 snacks
- shelter
- 99 cent store hygiene products
- medical
- the option to speak to a pre-licensed therapist
- transportation to and from court or school
- access to do laundry
- “wrap-around-services”
- “family team meetings”
If you look closely, these are all things that the CCLD is monitoring.
What happens when a youth goes to a residential treatment center?
They get bullied by staff and other children, restrained, property searched every day if they leave the facility without a staff member or searched if suspected of having contraband, under 24-hour lockdown supervision (or should I say, control or restriction), possess no privacy (even in the bathroom), and develop no real attachments as staff rotates from morning to evening, backend and front end shifts.
Experiencing congregate care, the child might be retraumatized through trauma reminders or triggers:
-
Trauma Reminder #1 Neglect
Stealing food into their room, because food is limited during meal times, locked up with a key lock, or monitored by staff. The child is responding to trauma triggers that staff is intentionally withholding food.
-
Trauma Reminder #2 Physical and Sexual Abuse
Any form of physical touch they receive is when they are being restrained by multiple staff at least two (one person per arm) or up to five (one person per arm, per leg, and head). The child is reacting to trauma reminders when they have been physically or sexually abused as the staff is aggressively or forcefully pinning them down to the floor.
-
Trauma Reminder #3 Emotional Abuse
Most of the children in congregate care have low self-esteem, are not involved in any after-school programs, have poor academic performance, and find it challenging to build relationships with other kids and staff at the facility. For example, the children were unable to form teams to play volleyball, baseball, or soccer—at least for the 13-16-year-old’s that I worked with. While other children who are the same age, but come from a loving home are able to play with other children, the kids at the facility were not able to. The adults in congregate care sense their low self-esteem and some direct care workers might exploit the child’s shame, fear, and anger. Which makes the child believe that they are inherently bad and that everything they do is wrong. Enticing them to become angry, disrespecting them through downgrading words and actions. The direct care staff used their low self-esteem to create fear or guilt in the child. The child before entering congregate care already felt broken, but by the time they leave the facility, leave feeling more angry and guarded. Reenacting and reminding triggers of when they were being emotionally abused, staff retraumatized the child and harmed them in their care by also being emotionally abusive.
-
Trauma Reminder #4 Psychological Trauma
Communicating with family, friends, social workers, foster care ombudsman or CCLD is never private. The phone is placed right next to where the staff monitors the hallway and living room area. Not only does their low worth affect their behavior. The child has difficulty knowing and describing internal experiences and emotions. Uncertain of the dependability to communicate with others like their social worker, direct care worker, the CCLD, or foster care ombudsman to help them with their problems, the children sometimes do not even try. And when they were brave enough to ask for help, the person they asked was unable to help them— justifying their internal belief that people are not to be trusted. Since the child is already scared of forming relationships, having more negative experiences communicating their needs, their complex trauma makes the therapist and client relationship already very challenging. So whether that’s in person or on the phone, when the child communicates their discomfort to their therapist or direct care worker it is difficult for them, because their trust has been broken. Whether that be from their current placement or their biological parents, their trauma affects them to speak out. Especially if their privacy and outside forms of communication are being monitored 24 hours a day.
I am not saying their angels, but have a little empathy in your heart to know where they are coming from. I can point and say it was the staff and therapist who was the problem because it was the staffs’ and therapist’s lack of communication, that made me write zero on the child’s point sheet for program participation: therapy. But as a direct care worker, observing my coworker’s and the therapist lack of communication—I would say was a bigger reflection on the lack of accountability and training we didn’t receive from the facility’s board of directors, chief program officer, director, and supervisors of a short-term residential therapeutic program. Blaming the child for not wanting therapy, because they lacked initiative or refused to talk to their therapist was not the whole picture. Therapists and direct care workers were not properly trained or held accountable for their quality of care. The patient who is a minor can’t be responsible to ask for help when it can be assumed. The children in congregate care have a history of disrupted attachments, and therefore have an attachment impairment that prevents them from seeking help.
Children with disrupted attachment histories (out of home placement, multiple changes of primary caregiver) have the following signs of impairments:
- Difficulty trusting others
- Uncertain about the reliability/ predictability of others
- Interpersonal difficulty
- Social isolation
- Difficulty seeking help
- Clingy, difficulty with separations
As direct care workers, we should have been trained to advocate for the children by being more intentional. In other words, if the residents won’t take the initiative, treatment counselors, I encourage you to ask the child, “It looks like you haven’t talked to your therapist all week. Would you like to talk to your therapist?” And therapists, what are you doing to get to know your clients?
The services provided to your clients are being scored, so the treatment counselors have to know when or not the children are talking to their therapist. The mental health services provided to the children in a 24-hour facility aren’t working, because the clinician, along with the resident hasn’t established a foundation of rapport. The tragedy here is that vulnerable and innocent children, who are more likely to be thrown out of society, aren’t getting the right help they need in treatment.
It’s easy to mark their point sheet zero because it’s hard to advocate, encourage or communicate with their therapist. Some therapists, won’t engage with the child if they don’t want therapy, but the time missed with the child can be used to build rapport. Many clinicians and treatment counselors, who enter higher levels of care, enter it with no concept, no perspective in what they are going to be encountering. It’s definitely a learning curve. What it takes for a person to be cut out to do therapy in an in-patient facility, in comparison to a community setting, the therapist will have to be in crisis mode more.
At the end of the day, they’re kids that no one else really wants to work with, but they are kids that have potential, and given the right tools I believe will be able to be successful on the outside. The point I am trying to make here is children who have been removed from their parents because they were unsafe, abused, neglected or their parents were unable to care for them, do not know how to ask for help! “If the people who were supposed to care for you, protect you, and love you unconditionally were the ones abusing and neglecting you, the message a kid receives is that people aren’t to be trusted, especially adults.”
Gap analysis
Treatment counselors it is your job to help your client get the best care and services, while you are here! And therapist it is your job to understand the effects of childhood trauma, dare I say, better than anyone else. Even though the kids we work with lack the skill to connect with us or those around them (yes, this can make our job feel almost impossible), this shouldn’t stop us from reaching out and doing our best for every child in our care! Children who are victims of abuse often experience poor social interaction (relationships with adults and peers), poor emotional awareness (the ability to recognize and understand their own feelings), and poor self-regulation (the ability to express thoughts, feelings, and behaviors in socially appropriate ways).
I hate to say this, but we have to remind ourselves why we are here. If that’s to just get paid or to get your supervised hours. Then this is not the right job for you. We are advocating for our resident’s best interest, which requires both the treatment counselor and therapist to care.
Developing a relationship between the resident and therapist.
- Treatment counselors it’s your job to develop a relationship with each of your residents and their therapist. This is how you can bridge the communication gap between the resident to their therapist.
- Therapist is your job to build a relationship between each of your clients and their treatment counselors. This is how you can bridge the communication gap between the adults who are working very closely with them—who can help assist in that transition by prompting or encouraging the resident to go to their therapy session.
Residents should also be provided advocating classes in order to ask for help when all else fails, such as when staff fails to do their job correctly. As an adult, I didn’t feel safe asking for help because of my toxic teammates. I can only imagine how the children felt. Safety is one of the most important considerations to be made when establishing a therapeutic environment. A way to test if the environment feels safe is to ask yourself: “Do you feel safe in the environment where you are working?” My answer: NO! Not because of the youth, but because of my coworkers, supervisor, and the chief program officer.
Engagement plan
Let’s define each part of the plan. The therapist your job is to be the transference parent. According to the STRTP organization I worked with, this is the clinician, who the child/resident will superimpose their parent relationship on, in order to attempt to address/ work through relationships.
Therapists when you are on duty build rapport with your client. Check-in on them and let them know:
- Who you are (i.e. “Hi! My name is_______. I am your therapist.”)
- What is your phone number or extension is (i.e. “Whenever you are feeling down or want to talk, you can reach me on this extension. If I don’t answer, leave me a voice message and I will get back to you as soon as I can.”)
- What’s your work schedule (i.e. “These are my work hours. Every time I am in, I will check in on you when I am available.”)
- And how you can help! (i.e. “I just want to remind you that this is part of your program. If we check in once a week, I can provide you with x,y,z.)
When therapists check in on their clients, get to know them.
- Spend time with them by observing client interaction with staff and peers.
- Ask open-ended questions:
o How has your experience been with therapy?
Tip: The tone should be warm and approachable. Tracking conversation, lets the client know you’re listening. Make eye contact and smile when it’s appropriate.
- Ask closed-ended questions:
- What are your interests?
- What are your hobbies?
- How was your day?
- What did you do?
Tip: Be willing to open up and share your interest as well, such as favorite music/TV show/ and subject in school. Be intentional and pick up the last conversation to let the client know you listened.
- Therapists can identify session rewards that are particularly meaningful to their clients, such as a favorite song, game, or activity (e.g., basketball) (Cohen et al., 2012).
- Take initiative and bring a card game of Uno and ask them to play or bring an art project and ask them to join you.
- Find out what’s their favorite snack or drink and bring it to them, the next time you check in.
- Invite residents into your office if you can and make it feel comfy and inviting!
- Follow up with a next appointment date
- Always keep your promises, because trust will be broken between the client and you.
- Accept and don’t pass judgment when they open up.
It is important that the clinician be genuine and actively engaged in the therapeutic relationship, feel empathy… and have unconditional positive regard for the youth. The therapeutic relationship and alliance are among one the key factors in treatment retention and success. Establishing rapport creates mutual respect between the clinician and youth in therapy, which can allow a therapeutic relationship to be developed and maintained. The therapist meets the resident’s specific needs by first developing a good rapport with their client. After building rapport, the client can ask the youth to prioritize his or her list of problems, making the client a part in creating their individualized treatment plan. Since the client was a co-creator of the treatment plan, the child might feel more motivated to delve right into therapy.
Treatment counselors, your job here is to be a caring parent. According to the STRTP organization I worked with, this is the treatment counselor, who provides for the basic needs of the child/resident. Ideally, each child/resident should have a primary who knows their kid “exquisitely.” In situations where there is no parent participating in treatment, the therapist can ask the child whether he or she would like to ask a specific milieu staff member to participate. (3) Treatment focused on making the child feel safe because their relationship with their caring parent (treatment counselor) was engaged and involved. And when a parent is actively participating in services, counseling outcomes are more successful.
- Treatment counselors introduce yourself to your client’s therapist (i.e. “Hi! My name is_______. I am the resident treatment counselor for the morning or evening/frontend or backend shift.”)
- Update the therapist on how the resident is doing for the day, week, or month.
- Share what you know: their triggers, strengths, interest, passions, or hobbies.
- Advocate for them when you observe an uncharacteristic change in their behavior.
- When the client has stopped eating.
- When the client has slept in their room all day.
- When the client has been unmotivated to do hygiene.
- Ask the therapist how you can help with the resident’s treatment plan. Asking:
- “Would you like me to model interventions?”
- “Would you like me to practice coping skills?”
- “Would you like me to role-play with the client?”
Most therapists in residential facilities are pre-licensed!
Treatment counselors and therapists having little to no experience at all, have to hit the ground running. Both are usually young, just graduating. Have no idea what they are doing when providing high levels of care to children in need. Pre-licensed therapists who are just starting off their careers usually have just graduated and are young themselves. I believe are too inexperienced to work in group homes or residential facilities. You can be young and have the experience, I just think therapists who work with special populations in STRTP or higher levels of care, need specialization in trauma therapies.
If a child is in a treatment center, you would think they would desperately need higher-quality mental care. And see a licensed clinician. Someone having completed their hours in supervised training and passing the National Physical Therapy Examination (NPTE), would greatly benefit the quality of care in residential treatment. A clinician specializing in dialectical behavior therapy, trauma-focused CBT, Aggression Replacement training or any other type of evidence-based treatment can also be beneficial. However, do you think places like this want to pay that much money?
Treatment counselors are untrained in trauma support!
Not only therapists, but direct care staff members are often young, have had little or no professional education about child psychopathology, and have little prior experience working with troubled children. These individuals receive annual mandated training in techniques for conflict resolution and management of problem behaviors, but because they are often spat on, called names, and kicked and/or punched by residents, they may take this personally, viewing themselves as victims of abuse by the children in the RTF (residential treatment facility) rather than seeing these children as reenacting trauma that they themselves have experienced (Cohen et al., 2012).
I believe treatment counselors can provide a higher quality of care, as long as they are getting the right type of training and accountability from the organization’s directors. Yet, how many facilities want to pay for the appropriate training when the turn-over rate in their perspective is fleeting. Treatment counselors are not trained in child care, coping skills, self-regulation, anger management, or trauma. Since direct milieu staff members’ task is to manage children’s problems in the RTF milieu, these workers must understand how trauma impacts children in RTF settings, how to minimize trauma reenactment in the milieu, and how to optimally support therapy implementation (Cohen et al., 2012).
Residential treatment facilities make behavioral, emotional, and substance abuse worse!
Many of the staffs’ biases, implicit and explicit biases need to be challenged. While in RTF, youth experience high rates of trauma exposure. But did my coworkers ever stop and wonder, taking into consideration how the potential influence of trauma can influence the resident’s behavior, emotional, and substance difficulties in RTF? I always questioned if the staff really cared about the youngsters they work for or if they were just there because they liked the feeling of being in charge. Treatment counselors who just graduated are now put into positions where they are literally over all these children. A lot of the staff, because they are young and aren’t used to that type of power, abuse it. It can really go to their head.
Having an open and accepting attitude for all persons coming to treatment will cultivate a positive therapeutic relationship, which will enhance the therapeutic environment. Out of the whole time I worked in RTF, I only got disrespected a couple of times. But I was also very respectful to the youth. When a child spits on, calls names, kicks, or punches, you only hear about what happened after—the cussing, name-calling, or shouting, but not what happened before—what the staff did to trigger the youth. You don’t know what the hell pushed that youth to do that. Maybe because they were getting treated like animals and animals bite back. Maybe the treatment counselor was talking shit to the adolescent or abusing their power. I believe some children who feel threaten or scared fight back, while others turn that rage inward so that it becomes depression or numbness. How a treatment counselor is treating that particular child based on prior expectations—accurate or not— might have an influence on how they’re reacting in turn. Even if that child wasn’t hostile, staff might have turned him into a hostile child by treating him in a way that elicited that hostile reaction from him. For example, when talking staff’s eyes might narrow when they talk to a child who comes to them with a certain request. The child acts respectfully, even waits patiently, but the staff doesn’t like him. Staff needs him to know he’s not going to respond immediately. He’s got to wait. The child reacts aggressively and justifies the staff’s self-fulfilling prophecy, even if those expectations were never voiced.
The therapeutic environment is a constructed idea created before, during, and after experiences where services are rendered relative to mental health care. By creating a therapeutic environment, a person will be more at ease when coming in for services and will be likely to be more comfortable talking about sensitive topics, such as trauma. If an effective therapeutic environment is established, a person will be more likely to be less resistant because there is a subconscious sense of safety. Creating a therapeutic environment takes a conscious and intentional effort by the clinician and by those responsible for the administration of programs. By creating a therapeutic environment, clinicians can support progress toward treatment goals, personal growth, and positive change for people seeking services.
Building rapport in a residential facility with clinicians feels scary.
The therapeutic environment is an essential consideration when evaluating best practice for clinicians that are working with children who have health and/or mental health needs. The therapeutic environment is a factor well before a child is seen for services. In fact, as soon as a child comes into the lobby or other space, the environment has an impact on how the child will perceive the experience.
With little accountability and training, treatment counselors set the culture and tone of a group home or institution’s quality of care. When you have a lead counselor, unit manager, assistant director, director, and chief program officer who is a bully, the ripple effect goes down. If treatment counselors have a bad attitude, that affects the children who have to live and survive in that treatment center. According to the American Psychological Association’s Dictionary of Psychology, a therapeutic atmosphere is, “an environment of acceptance, empathetic understanding, and unconditional positive regard in which persons feel free to verbalize and consider their thoughts, behaviors, and emotions and make constructive in their attitudes and reactions.” When a person comes into a therapeutic environment, they should have a pleasant, beneficial experience.
And we wonder why foster children who turn 18 or 21 suffer from anxiety or other stress-related disorders.
“Youth who live in institutional settings are at greater risk of developing physical, emotional, and behavioral problems that can lead to school failure, teen pregnancy, homelessness, unemployment, and incarceration and are less likely to find a permanent home than those who live in family foster care.”
Because they spent the last 2 years (sometimes more) give or take in congregate care getting picked on or having to adapt to survive in a restrictive institution. The mental services provided by the program didn’t help the client’s behavior or emotional problems. If anything they made them worse! The program couldn’t provide the type of environment where the child felt safe to open up in therapy because the child had to worry not only about the other kids picking on them but some staff who were out to get them. Creating an environment where a sense of security or safety was just a fake pretense. The atmosphere was not warm or inviting through the building. It was hostile. Where microaggressions were unknowingly and inappropriately delivered by the helping professional.
Why a high turnover rate of therapists and residential counselors can affect the child’s treatment!
According to the research paper, Causes and Solutions for High Direct Care Staff Turnover, “High turnover rates could be detrimental to residents’ mental health and well-being because continuity of care and personal relationships with the staff tend to be important for this population, are disrupted. Often these clients grieve the loss of some of their closest staff members and as a result, have difficulties establishing trusting relationships with the new staff members.
When the leadership is bad, you don’t have to wonder why the staff turnover rate is so high. One of the biggest reasons people are miserable in their work has nothing to do with the job itself. Being a treatment counselor or therapist, you might be in your sweet spot, doing the thing you love, but were in an environment of toxic leadership and toxic teammates. I don’t know anyone who wants to go to work every day and deal with difficult people—even if you loved the children you worked with. Bad leadership affects the staff as much as it affects the youth because we all experienced the same things. The only difference was, we were able to go home.
Why staff might leave?
According to a 2010 study completed by the National Institute of Health, “In some cases, the pool of workers is inadequate to handle the current client demand, coupled with inadequate training and work stress which can diminish the effectiveness of care delivered.” Tasks now encompass motivating clients on skill development, providing personal care… medication administration, and personal grooming.
- Staff feel inadequately compensated for the work they do
- Staff feels they receive insufficient support from their supervisor.
- Staff feels the training they received to work independently as a direct care worker was insufficient.
What’s really the best treatment setting for children?
Therapy can be conducted in private practice offices, clinics, counseling centers, and community spaces, as well as in facilities, and in homes and other community-based locations. Trends in psychotherapy are, in some cases, moving towards home and community-based practice. Why?
- The three main benefits of home and community-based care versus institutional care are cost-effectiveness, more treatment options, and better care of the individual.
- In regards to the therapeutic environment in home-based therapy, the therapeutic relationship may form more quickly in home-based therapy.
- The individual receiving therapy is usually more comfortable and relaxed because they are in their own environment.
The truth is, home and community-based care is the best treatment setting for children. Every child is worthy of a loving family, and should not be placed in congregate care, simply because it’s easier to house a child or teen there. In fact, more than 40 percent of these children have no documented clinical or behavioral health need that would indicate a placement outside a family setting, and still many children, especially teens, end up in restrictive settings while in care. Finding teens a home is difficult, but the reality is, all children deserve to be raised by adults who love and who are communicating that love to the child. They’re not focused on controlling the child but are role modeling the appropriate behaviors the child can emulate. The child who is still struggling with their mental health diagnosis can receive outpatient therapy, while also living in a home.
Work Cited
- Foster care and Homelessness
- Miriam Aroni Krinsky, Disrupting the Pathway from Foster Care to the Justice System—A Former Prosecutor’s Perspectives on Reform, 48 Fam. Ct. Rev. 322, 325 (2010)
- Study Finds Foster Kids Suffer PTSD
- Trauma Signs and Symptoms
- What is Foster Care?
- Why do some people who experience trauma as children have difficulty asking for help?
- Child Abuse
- Cohen, J.A., Mannarino, A.P., & Deblinger, E. (2012). Trauma-focused CBT for Children and adolescents: Treatment Applications. New York, NY: Guilford Press.
- Best Practice for Therapeutic Environments: A Guide for Clinicians and Administrators
- Implementing Evidence-Based Practice in Residential Care-How Far Have We Come?
- What are the Outcomes for Youth Placed in Congregate Care Setting?
- Causes and Solutions for High Direct Care Staff Turnover
- Every Kid Needs a Family: Giving Children in the Welfare System the Best Chance for Success